If you are constantly feeling bloated and with digestive issues, you are not alone. Digestive health is a crucial component of overall health and wellness. The problem is that it’s often overlooked.
For those struggling with digestive conditions, such as Irritable Bowel Syndrome (IBS) or Small Intestinal Bacteria Overgrowth (SIBO), finding relief can seem daunting.
If you feel you are alone in this journey, rest assured that you are not. Research shows that over 7-18% of the population has IBS. The most shocking statistic is the connection between IBS and SIBO. Research shows that over 35% of people with IBS also have SIBO.
If you’ve already been diagnosed with one (or more) of these conditions, chances are you’ve heard of the low-FODMAP diet. Many doctors today recommend the low-FODMAP approach to new patients.
And while we at CanXida aren’t huge fans of the low-FODMAP approach (for reasons we’ll explain in a moment) we do recognize its value & usefulness for many patients, as long as it’s followed correctly.
The low-FODMAP diet can help you discover which foods in particular are triggering your flare-ups, but it is not a long term solution to IBS or SIBO and shouldn’t be used as such.
And that is because of how restrictive it is. It takes almost all carbohydrates out of the diet. Remember, we shape our microbiome & gut bacteria by what we eat. So the more restrictive you are with food, the more restrictive the bacteria will become in the gut.
And over time this can create dysfunction. It can create a situation where if you deviate off it, you’ll get sick rather quickly. Which of course will make you think “I need to get back on the FODMAP diet.”
We’re not saying you shouldn’t try the low-FODMAP approach if you’re struggling with IBS, SIBO or another gut issue. By all means, give it a shot. It’ll probably help you. Just don’t make the mistake of thinking you need to stick to it for months or years.
And with that out of the way, let’s dive into what the low-FODMAP diet is, what foods are allowed, and how to add supplements to it so you get better results faster.
What Is the FODMAP Diet? & How Does the FODMAP Diet Work
FODMAPs stand for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These short-chain carbohydrates are resistant to digestion.
So, instead of being absorbed into the bloodstream, they reach the far end of your intestine where most of the gut bacteria reside. While they may offer some benefits to some, for others, it may cause serious digestive problems.
But why can they cause digestive problems?
FODMAPs draw liquid into the intestine and become fermented by the bacteria, leading to gas, bloating, and pain. This process can affect bowel movements and contribute to symptoms associated with IBS and other related gastrointestinal disorders.
Understanding which foods are high in FODMAPs is the first step towards helping manage these symptoms. However, it’s important to understand that the low FODMAP diet is not a one-size-fits-all approach. It is typically recommended as a temporary measure to identify personal triggers and should be followed under guidance of a healthcare professional.
The low-FODMAP diet categorized foods based on their FODMAP content, recommending the avoidance of those high in these fermentable carbs.
But which are the foods you should avoid?
Before we give you the list of foods to avoid, we strongly recommend you watch the video below, where we discuss 10 important things to know about the FODMAP diet. This will help you significantly and save you a lot of time in research and mistakes to avoid.
Here are some common high-FODMAP foods to be mindful of:
- Oligosaccarides (fructans and galactans): artichokes, asparagus, beetroot, Brussels sprouts, broccoli, cabbage, garlic, onions, leeks, shallots, wheat, rye, barley, lentils, chickpeas, cashews, and pistachios.
- Disaccharides: milk and any derivatives (yogurt, soft cheese, ice cream, custard, milk powders, and buttermilk.
- Monosaccharides: apples, pears, mangoes, watermelon, cherries, blackberries, nectarines, figs, honey, high-fructose corn syrup, and agave nectar.
- Polyols: apples, pears, blackberries, peaches, plums, sorbitol, mushrooms, cauliflower, and snow peas.
On the other hand, here are some low-FODMAP foods you want to focus on since they are less likely to cause any digestive discomfort.
- Proteins: chicken, eggs, fish, pork, turkey, tofu (firm), tempeh, and beef.
- Fruits and vegetables: bell peppers, carrots, cucumber, eggplant, green beans, lettuce, spinach, zucchini, tomato, potato, sweet potato, blueberries, kiwi, oranges, grapes, strawberries, pineapple, cantaloupe, and papaya.
- Dairy: lactose-free milk, hard cheeses, Greek yogurt, butter (small amounts), lactose-free yogurt.
- Fats and oils: chia seeds, pumpkin seeds, sunflower seeds, walnuts, olive oil, coconut oil, and peanut butter (natural and small amounts).
- Cereal, grains, and starches: gluten-free grain, oats, quinoa, rice, rice cake, cornflakes, popcorn (natural), and polenta.
This list is not exhaustive, and sensitivity to these foods can vary from person to person. The low-FODMAP diet involves a strict elimination phase, removing all high-FODMAP foods followed by a gradual reintroduction. But we are going to dive more in this later in the article.
Benefits of the FODMAP Diet
There are several benefits to following a low-FODMAP diet. Here are some of the benefits you may obtain.
1. Symptom relief for IBS & SIBO
The primary benefit of a low-FODMAP diet is the relief of symptoms associated with IBS & SIBO. Multiple studies have shown that people with IBS & SIBO who follow a low-FODMAP diet experience a reduction in symptoms.
In fact, a 2016 study showed that over 86% of people with IBS had a decrease in their symptoms when following a low-FODMAP diet.
2. Improved Quality of Life
Beyond symptom relief, people adhering to a low-FODMAP diet often report an overall improvement in quality of life. The decrease in uncomfortable symptoms allows for greater participation in social activities, reduced anxiety surrounding food and eating, and an overall sense of wellness.
A 2019 study found that people following a low-FODMAP diet not only has an improvement in their digestive symptoms, but it helped reduce fatigue, anxiety, depression, and increased happiness and vitality.
3. Enhanced Understanding of Food Triggers
Another significant benefit of following a low FODMAP is the enhanced understanding of personal food triggers.
While the diet typically beings with a strict elimination phase, it it followed by a gradual reintroduction, allowing you to better understand what foods trigger your symptoms. This can allow you to have a tailored and sustainable dietary approach that maintains rymptom relief while maximizing nutritional intake.
4. Support For Other Digestive Disorders
While a low-FODMAP diet is recommended for IBS & SIBO, evidence suggests that it may also be beneficial for people with other digestive disorders.
For example, it may seem beneficial for those with certain cases of inflammatory bowel disease (IBD). However, more research is still needed since they are still mixed results.
How to Follow the FODMAP Diet
Following a low-FODMAP diet may sound complicated, but, in fact, it’s quite simple. It only consists of only three phases. Here, we’ll go over each phase. But before we begin, remember to always speak with a health professional to have a tailored plan.
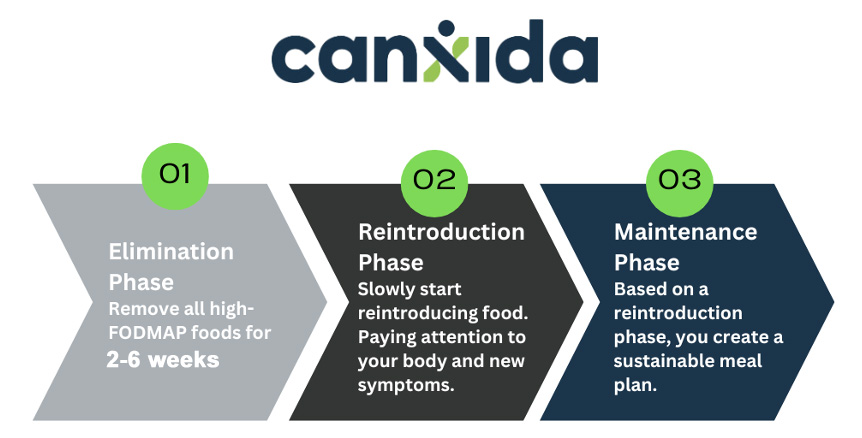
Phase 1: Elimination
The elimination phase involves removing high-FODMAP foods from your diet, which is crucial for identifying which foods trigger your symptoms. This phase shouldn’t last more than 2-6 weeks.
Practical Tips for the Elimination Phase
- Educate yourself. Before starting, familiarize yourself with high-FODMAP foods to avoid and low-FODMAP alternatives.
- Read labels carefully. Many processed foods contain high-FODMAP ingredients. Become a label detective and look out for hidden sources of FODMAPs.
- Keep it simple. Focus on simple, whole foods that are naturally low in FODMAPs, such as eggs, meats, certain vegetables like carrots and cucumbers, and fruits like bananas and oranges.
Phase 2: Reintroduction
After the elimination phase, you’ll slowly reintroduce high-FODMAP foods back into your diet, one group at a time. This helps identify which specific foods or FODMAP groups cause your symptoms and in what quantities.
Practical Tips for the Reintroduction Phase
- Introduce gradually. Add one food or FODMAP group back into your diet at a time, giving each trial a few days before trying another. This helps pinpoint exactly what triggers your symptoms.
- Keep a food diary. Document everything you eat and any symptoms you experience. This can help identify patterns and specific food sensitivities.
- Listen to your body. Everyone’s response to FODMAP is unique. Pay close attention to how your body reacts during this phase.
Phase 3. Maintenance
Based on your findings from the reintroduction phase, you will want to create a personalized low-FODMAP diet plan that avoids your triggers while maintaining nutritional balance.
Practical Tips for the Maintenance Phase
- Balance is key. Ensure your diet remains naturally balanced. Consider consulting a dietitian to help incorporate a wide range of foods into your diet.
- Stay flexible. Your tolerance to certain FODMAPs may change over time. Be willing to adjust your diet as needed.
- Explore new foods. Keep your diet interesting by experimenting with low-FODMAP recipes and foods you haven’t tried yet.
Managing Symptoms with the FODMAP Diet
Adhering to the FODMAP diet can significantly reduce symptoms like bloating, gas, and abdominal pain. As we’ve seen, taking away the foods that are causing you stomach disturbances can give your digestive system a break.
While diet alone can be a great way to help reduce IBS & SIBO symptoms, dietary supplements, can be a complementary approach. Many have found that combining a low-FODMAP diet with CanXida supplements leads to even greater benefits from digestive discomfort.
Dietary Supplements
If you’re looking for a supplement formula that works great with the low FODMAP diet, check out our range of supplements at CanXida. Our products are designed to support digestive health, making them an excellent complement to the low FODMAP diet. CanXida supplements are free from common allergens and irritants, ensuring they don’t exacerbate symptoms associated with SIBO, IBS and other gut issues. They contain carefully selected ingredients that aid in reducing inflammation, balancing gut flora, and promoting overall gut health, which is essential for those following a low FODMAP regimen.

Here is how they can support you:
- CanXida Remove: This all-natural, broad-spectrum antifungal, antibacterial, and anti-parasitic formula is designed to support a balanced gut flora.
- CanXida Restore: Contains probiotics and enzymes to aid in digestion and nutrient absorption.
- CanXida Rebuild: A comprehensive multivitamin that supports the immune system and gut health.
In combination with a low FODMAP, CanXida can help restore your gut health, allowing you to have better digestion. As a result, you may experience a reduction in digestive issues like bloating, stomach cramps, and better bowel movements.
Tips for Success on the FODMAP Diet
To make this journey as seamless as possible, here are some of the best tips we can provide you to have success following a low FODMAP diet.
- Start with professional guidance. Consulting a dietitian or healthcare professional knowledgeable about the low FODMAP diet is a pivotal first step. They can provide personalized advice, ensuring your nutritional needs are met while adhering to the diet’s restrictions.
- Plan your meals. Meal planning is your best friend on a low-FOMDAP diet. It prevents the last-minute scramble that often leads to poor choices. Dedicate time each week to plan your meals, relying on low-FODMAP recipes that excite your palate and keep things interesting.
- Create a low-FODMAP pantry. Stock your pantry with low-FODMAP staples, such as gluten-free grains, lactose-free dairy or alternatives, and low-FODMAP condiments and spices.
- Keep a food diary. A food journal can be an invaluable tool to help you track your meals, symptoms, and overall well-being. You can use our Candida Cleanse tracker to help you keep track of your symptoms. Although the title says “candida” the journal works perfectly fine for those with SIBO & IBS trying FODMAP diet.
Conclusion
A low-FODMAP diet can be a great approach to help you manage your digestive issues, such as IBS or SIBO. Combining the low-FODMAP diet with CanXida dietary supplements can offer you a promising approach to managing digestive discomfort.
By understanding and implementing the dietary changes and supplement strategies, you can take significant strides toward improving your digestive health.
If you are ready to transform your digestive health, consider exploring CanXida’s range of supplements. Together with a tailored FODMAP diet, CanXida can help you achieve the relief and wellness you’ve been seeking.
Frequently Asked Questions
Here are some questions that we get asked most of the time.
How Do I Improve Tolerance to FODMAPS Foods?
This is one of the questions we get asked most frequently. To help you better understand how to improve tolerance to FODMAP foods, we have created a video that we highly recommend you watch below.
Why are FODMAPs difficult to digest?
FODMAPs are types of cabs that are not fully absorbed in the gut, leading to fermentation by bacteria and resulting in gas, pain, and discomfort. Their poor absorption is why some people find FODMAPs difficult to digest.
Are FODMAPs bad for everyone?
No, FODMAPs are not bad for everyone. While they can cause issues for individuals with IBS or similar gastrointestinal disorders, many people can digest FODMAPs without any problems.
Who might benefit from a low-FODMAP diet plan?
Individuals with IBS, SIBO, or other gastrointestinal disorders may benefit from a low-FODMAP diet as it can help manage symptoms and improve quality of life.
What can I eat on the low-FODMAP diet?
On a low-FODMAP diet, you can eat foods low in FODMAPs, such as certain fruits like bananas and blueberries, vegetables like carrots and spinach, gluten-free grains, lactose-free dairy products, and proteins like eggs, tofu, and certain meats.
Which high FODMAP foods are the best to avoid?
High FODMAP foods to avoid include onions, garlic, wheat-based products, dairy products high in lactose, and certain fruits like apples and pears, and legumes.
What should I do before starting the low-FODMAP diet?
Before starting a low-FODMAP diet, consult with a health professional or dietitian to ensure it’s appropriate for you and to receive guidance on how to implement the diet effectively.
How long should I stay on a low-FODMAP diet?
The elimination phase of the low-FODMAP diet typically lasts 2-6 weeks. After this, foods are gradually reintroduced to identify triggers. The duration can vary based on individual responses and should be guided.
What if it doesn’t work for me?
If the low-FODMAP diet doesn’t alleviate symptoms, consult with a health professional for further evaluation. Other dietary strategies may be required.
How do you find FODMAP food triggers?
Finding FODMAP food triggers involves systematically reintroducing high-FODMAP foods back into your diet after the elimination phase to identify which ones provoke symptoms.
What are the differences between a low-FODMAP diet and a gluten-free diet or dairy-free diet?
A low-FODMAP diet restricts foods high in certain fermentable carbs, while a gluten-free diet eliminates all forms of gluten. On the other hand, a dairy-free diet excludes all dairy products. The low-FODMAP diet may include gluten or dairy if they are low in FODMAPs.
What are the best low-FODMAP snacks?
Best low-FODMAP snacks include a small serving of low-FODMAP fruits, lactose-free yogurt, gluten-free crackers with cheddar cheese, and small portions of nuts like walnuts or pecans.
Is the FODMAP diet permanent?
No, the low-FODMAP diet is not meant to be permanent. It’s a temporary elimination diet to identify dietary triggers, after which many foods can be reintroduced into the diet.
Does it help with IBS? How?
Yes, the low-FODMAP diet helps many people with IBS by significantly reducing dietary triggers that cause symptoms like bloating, gas, and stomach cramps.
Does it help with constipation? How?
The low-FODMAP diet can help some individuals with IBS-related constipation by stabilizing digestion and reducing bloating. However, it’s important to ensure adequate fiber intake.
Are there any risks with a low-FODMAP diet?
While the low-FODMAP diet is generally safe, there is risk of nutritional deficiencies if the diet is not well planned or if it’s carried out for too long without professional guidance.