Author: Dr. Blake Myers
Table of Content
Introduction
The Role of the Microbiome in Health and Disease
- The Early Years
- Maintenance of the Gut Barrier
- Protections from Infection
- Immune System Regulation
- Enhanced Nutrient Absorption
- Vitamins and Other Important Chemical Production
- The Gut-Brain Axis
Eubiosis vs. Dysbiosis
- Poor Diet
- Antibiotic Use
- Other Medications
- Chronic Stress
- Specific Dietary Factors
- Excessive Hygiene
- Alcohol Consumption
- Immune Suppression
- Gut Infections
Recognizing Signs of Dysbiosis
Dysbiosis and Its Impacts On Health
Resolving Dysbiosis: Effective and Holistic Strategies
I. Introduction
The Gut Microbiome: Your Body’s Hidden Ecosystem
Inside your gut there is a complex ecosystem of living organisms, living separately but in concert with your own body’s cells. The health and well-being of this microbial ecosystem is as equally important to your overall health as any collection of cells and organs of your body.
Research over the past ~20 years has demonstrated the intimate connection between the composition of your microbiome and your health. We now know that regardless of the disease or dysfunction, the health of the gut and the microbiome within cannot be ignored.
Picture this – trillions of cells – bacteria, fungi, parasites, and even viruses – equaling and possibly outnumbering the cells of your body…
Each one of these, taking up its own real estate, hanging out with others whom it works well with, fighting off those it doesn’t – all the while regulating and influencing the function of every biological system in your body. The impacts are fascinating and profound.
Not surprisingly, maintaining the health and balance of this gut microbial ecosystem is a huge topic with a great deal of complexity and considerations.
Dysbiosis – the imbalance of the bacteria in the gut – is one of the key aspects to understand if you want to optimize your gut health and maintain robust wellness.
This article is a comprehensive guide to dysbiosis, how to recognize it, and how to resolve it for good!
While organisms like Candida live in the gut and can cause many health issues, this article will focus primarily on the bacteria present in the gut.
If you want to understand all about Candida overgrowth in the gut, we have a comprehensive webinar you can watch that will teach you everything you need to know to recognize it and address it using our holistic protocol.
II. The Role of the Microbiome in Health
The Early Years
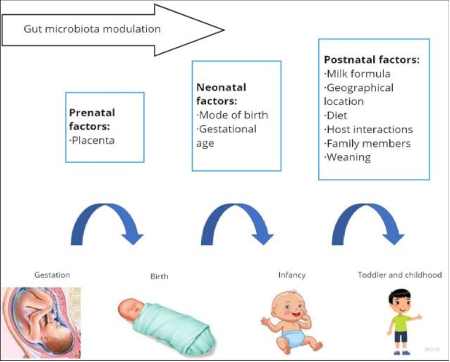
The human digestive tract gets inoculated in utero with microbes and then further colonized with additional strains at birth. In a vaginal delivery, the mother’s natural flora is the first major source of bacteria present. The vaginal microbes colonize and inhabit the mouth and digestive tract of the infant.
In cesaraen (C-section) birth, the exposure to the vaginal microbiome is absent and instead the first microbial exposure is that of the skin and a hospital environment. Research has demonstrated that the microbiome developed from cesarean delivery may contribute to some health outcomes later in life, such as allergies, asthma, diabetes, and obesity.
While better health outcomes have been correlated to the type of delivery, vaginal being optimal, there is much more that contributes to the quality of the microbiome beyond this first exposure.
The type of feeding an infant receives also has a large impact on the number and diversity of bacteria in the early infant gut. Breast milk contains prebiotics, specifically human milk oligosaccharides (HMO). Breastfeeding also plays a central role in “seeding” the infant gut with bacteria derived from the breast milk itself.
Prebiotics act as a primary food source for healthy gut bacteria and serve to build up robust numbers in early life. Formula fed infants miss out on this particularly important form of microbiome building support and may do well with intentional prebiotic supplementation.
Al-Rashidi HE. Gut microbiota and immunity relevance in eubiosis and dysbiosis. Saudi J Biol Sci. 2022;29(3):1628-1643. doi:10.1016/j.sjbs.2021.10.068
In addition to these modulating factors, significant influences on the microbiome in childhood and throughout life include environmental factors such as with whom you cohabitate, having pets, and geographical location.
A child’s microbiome is relatively formed to it’s adult stage by the age of 3. While it is completely possible to manipulate the gut flora composition throughout life, it is somewhat set to what it will be in the future without major altering influences present.
The infant immune system is new to the world and a fundamental role of the increasing numbers of gut bacteria is to educate and build up the immune system. These gut bacteria literally help form the immune system in early life and depending on the type and numbers of gut flora present, a variety of immune system related outcomes may ensue.
One outcome is a robust and balanced immune system function. This child will have a vital and appropriate response to infections and environmental exposures.
With a dysbiotic gut microbiome, a child is likely to have some level of immune system dysregulation. Commonly, these children are more prone to develop allergies, food sensitivities, atopic dermatitis (eczema), and asthma, among other conditions.
These childhood manifestations of an imbalanced immune system often change over time. For example, asthma may go away, but the remaining core issues may contribute to autoimmunity or generalized chronic inflammation in adulthood.
This is important to recognize because chronic inflammation underlies the majority of chronic illness we deal with in modern society.
Maintenance of The Gut Barrier
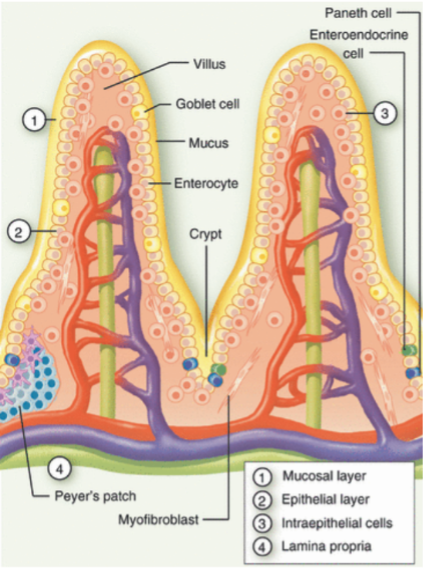
One of the primary roles of the gut is to form a selective barrier between you and the outside world. You may think of your digestive tract as being inside your body. This makes sense, but in actuality, it is a tube that is in constant contact with the outside world. Your skin, lungs, and digestive tract are the largest areas of contact with the outside world.
The gut lining is only one cell layer thick. Just on the other side is the blood stream and a great deal of immune cells. For this reason, it is essential for health and survival to allow only specific molecules and particles across the gut barrier.
Moens E, Veldhoen M. Epithelial barrier biology: good fences make good neighbours. Immunology. 2012;135(1):1-8. doi:10.1111/j.1365-2567.2011.03506.x
The gut barrier is kept intact largely through five mechanisms.
- Mucus layer
- Immune system defense
- Microbial barrier
- Tight junctions (TJ)
- Paracellular transport
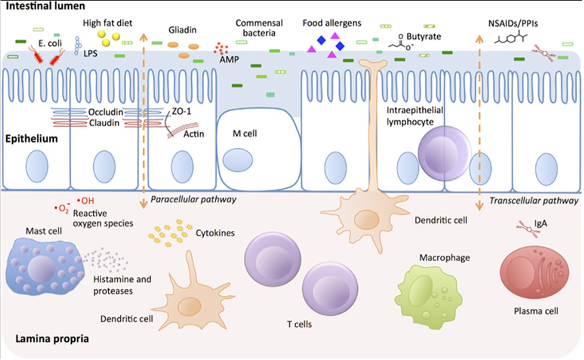
The mucus layer provides a physical barrier between the intestinal cells and contents of the digestive tract. When bacteria, other microbes, or toxins get too close to the gut wall, it can trigger inflammation and a breakdown of the selectivity of what is allowed across the gut barrier.
Healthy gut bacteria produce a primary byproduct called butyrate that is responsible for stimulating intestinal cell mucus production. Without butyrate, intestinal permeability or “leaky gut” is likely to ensue.
Seeing as 95% of all infections enter through mucus membranes, gut mucus lining is a required part of protection from a variety of infections.
The other way the cells of the gut lining keep microbes from getting too close is through producing antimicrobial peptides (AMP). These form an additional barrier by killing those that come too close. Healthy gut bacteria, again through butyrate production, promotes the production of these beneficial AMP’s.
Between the cells are tight junctions (TJ). TJ’s are like gates between the intestinal cells that are so tight, they keep water from passing through when closed. The TJ’s are supposed to open and close selectively but for many reasons, they can become dysfunctional. This is what is usually referred to as “leaky gut”. Inflammation is a primary trigger for TJ function to break down. The microbiome prevents inflammation in multiple ways, the physical barriers already mentioned being two. It also supports the maintenance and reassembly of health TJ’s.
The last pathway for a “leaky gut” is straight through the cells themselves. This is called transcellular transport (TT). TT is vital to getting appropriate substances into the body and it is highly specialized. Pathogenic bacteria can interrupt this specialization and cause this pathway to dysfunction. The healthy gut bacteria are a central mechanism to defend against gut pathogens through forming what is called a microbial barrier (MB).
The MB is literally the microbes themselves taking up real estate and not wanting to give it up. Bacteria have ways of fighting others off, such as by making antimicrobial compounds. The presence of large numbers of healthy gut bacteria will promote the maintenance of the ecosystem, while imbalance more easily allows pathogens in.
Protection From Infection
Within the digestive tract, there is only so much space and resources available. Not unlike humans, once bacteria and other microbes have a comfortable home and plenty of food available, they do not want to give up this niche and will not relinquish it easily.
Take the fungi Candida for example. In 40-80% of people, Candida species are a normal part of the gut microbiota. One benefit to the presence of Candida at healthy levels is it protects against the colonization and proliferation of serious infections from species such as Clostridium difficile (C. diff) and Pseudomonas aeruginosa.The Candida don’t want to give up their prime living space to these invaders. Bacteria work similarly.
Microbes hold their space and fight off colonization with other organisms by:
- Using the nutrients present so pathogens can’t grow
- Preventing pathogens from having a space to inhabit
- Producing antimicrobial compounds to kill pathogens
Immune System Regulation
70-80% of your immune system lies in your gut. Recognizing this, the health of your gut, the microbiome, and the nature of what signals you’re giving your immune system through what you’re putting in your body, are vital aspects of overall health.
Your microbiome trained your immune system from infancy and helps keep it robust today. In addition, the bacteria in your gut help to regulate your immune system – keeping a healthy balance between activation and standing at the ready.
Many of the previously mentioned mechanisms involved in the maintenance of the gut barrier are considered part of your innate immunity. Innate immunity is your first line of defense against pathogens.
The other branch of the immune system is called adaptive immunity. Adaptive immunity responds to foreign “invaders” – including chemicals and other toxins – and leads down a path of specific reaction to address each. This is the pathway that gives us immune system memory of certain infectious organisms, and also actively attacks and kills non-self substances, such as bacteria and viruses.
In the adaptive immune system, there are what are known as Th1 cells and Th2 cells. Ideally, there is somewhat of a balance between the two. Commonly, a predominance of Th1 cells are associated with inflammation and autoimmune disease. Th2 are typically associated with allergic and atopic conditions, like eczema, asthma, and environmental allergies.
A healthy gut microbiome supports a balance of Th1 and Th2 throughout the entire body by stimulating T regulatory (Treg) cells. These cells literally regulate if T cells stay quiet, or if they go down one or the other pathway. Healthy Treg cell populations are foundational to a strong, yet balanced immune system response.
There are also specialized immune cells inside your intestinal cells, called intraepithelial lymphocytes (IEL). These are a primary defense against gut infections. IEL’s are kept healthy and functional by the presence of a healthy gut microbiome.
Enhanced Nutrient Absorption
Your digestive tract is an expertly evolved system for the breakdown and absorption of nutrients from food. Both steps are necessary in order for the foods you eat to enter your body and be used for energy and as building blocks. It turns out that your body is not alone in it’s efforts to optimize these processes of nutrient breakdown and absorption.
Bacteria are able to help break down nutrients into small enough components that they can be absorbed. Amazingly, gut bacteria also regulate the absorption of nutrients. In particular, vitamins and minerals.
Enzymes produced by bacteria help release vitamins and minerals that are bound and require release from other dietary products and then subsequently control the rate of absorption so that they can also receive what they need.
Production of Vitamins and Other Important Chemicals
Bacteria have the ability to make numerous substances as byproducts of their metabolism. Butyrate, a short-chain fatty acid (SCFA) mentioned multiple times in the gut barrier maintenance section, is an example of a beneficial byproduct produced by a variety of healthy gut bacteria from fermentation of fiber.
One way beneficial gut flora directly support our health is by producing vitamins. Vitamins produced include:
- Vitamin K
- Vitmain B1 (thiamine)
- Vitamin B2 (riboflavin)
- Vitamin B3 (niacin)
- Vitamin B5 (pantothenic acid)
- Vitamin B6 (pyridoxine)
- Folate
- Biotin
- Vitamin B12 (cobalamin)
These give a significant supplemental increase in addition to dietary intake if you maintain a healthy and diverse microbiome.
Your gut bacteria also produce and contribute to the production of neurotransmitters and hormones. These don’t just stay in your gut but are absorbed into your bloodstream. Through this and other mechanisms, your gut microbiome has a significant impact on your total body physiology and mental health.
The Gut-Brain Axis

Strandwitz P. Neurotransmitter modulation by the gut microbiota. Brain Res. 2018;1693(Pt B):128-133. doi:10.1016/j.brainres.2018.03.015
The gut-brain axis is a bi-directional network in where the brain and the gut“speak” to each other. For the purposes of this section, we are concerned only with the impact of the gut on the brain.
As was already mentioned, the gut microbiome can impact the brain through modulating neurotransmitter and hormone levels. Many vitamin and minerals modulated by bacteria also have significant effects on brain health.
Beyond the biochemistry of the interactions, there is a neurologic highway connecting the gut and the brain – the vagus nerve.
The vagus nerve innervates the first ⅔ of the digestive tract and the associated organs such as the pancreas and stomach. The vagus nerve controls the activities of the rest and digest functions. When the vagus nerve is appropriately stimulated, digestion functions optimally.
It’s also true in the opposite direction. When the digestive system is functioning properly, the vagus nerve sending signals from the gut to the brain is sending what can be broadly considered “healthy” messages.
Vagus nerve “tone”, as it’s called, is associated with lower systemic inflammation and a calmer state of being. Perhaps most importantly, altered vagus nerve function is associated with serious diseases such as Parkinson’s disease. Electrical stimulation of the vagus nerve is currently considered a potential therapeutic option for neurodegenerative diseases like Alzheimer’s.
The microbiome plays a primary role in natural stimulation of the vagus nerve. This is likely one major reason that the microbiome and the gut-brain axis are considered by many to be at the root cause of the development of neurodegenerative disease.
This image illustrates many aspects described in section II.
III. Eubiosis vs. Dysbiosis
This section will define eubiosis and dysbiosis, followed by the impact of dysbiosis on health.
Eubiosis
Eubiosis is an interspecies balance among microbes in a community. This means when there is a balance of the bacteria, fungi, and other organisms in your gut – collectively called the microbiota – there is a sort of homeostasis that happens.
In gut eubiosis, all of the organisms have relatively all the space, food, and nutrient sources they need to live healthily. Within a eubiotic gut flora environment, the microbes also typically have other species around that they live well with. There are many mutualistic and symbiotic relationships.
With beneficial bacteria thriving in this state of balance and harmony, they contribute to the various physiological processes essential for maintaining overall health, which were discussed in detail in the previous section.
Dysbiosis
Dysbiosis is a result of the disruption of eubiosis. Since eubiosis is a balance in a microbial ecosystem, gut dysbiosis can be thought of as an imbalance in the composition – and also the function of – the gut microbiome.
Dysbiosis has a variety of presentations and individual variations.
Imbalances seen in dysbiosis can be:
- Lack of microbial diversity
- Low numbers of gut microbes
- Overgrowth of one or more specific microbes
Commonly, dysbiosis results in one or a combination of these dysbiosis patterns. There can be low numbers and low diversity, for example. A typical pattern is too many problematic microbes and simply not enough good ones.
While bacteria are typically imbalanced in some way in dysbiosis, it is important to remember that issues like Candida overgrowth are also dysbiosis issues and should be addressed appropriately.
You can access CanXida’s free clinical protocol if you need guidance with this.
V. Common causes of dysbiosis
Dysbiosis can be caused by one strong causative factor. However, more often it is a result of a variety of contributing factors that lead to true dysbiotic issues. Clinically I have seen dysbiosis and issues such as small intestinal bacterial overgrowth (SIBO) happen after one round of pharmaceutical antibiotics. Even in these cases though, there is usually a history of predisposing factors that primed the system for a poor outcome.
These are the most common causes of bacterial dysbiosis in the gut. The more of these variables are out of balance, the greater your chances of developing dysbiosis, and the more difficult it will be to resolve as long as they remain unaddressed.
Poor Diet
In the United States, researchers describe what is commonly referred to in the literature as the Standard American Diet (SAD). This primarily consists of many processed and ultra-processed foods, high in salt, sugar, inflammatory fats, and low in nutrient density. Most Americans also do not get the recommended amount of fruits and vegetables in a day. This leads to one of the most damaging characteristics of a SAD, the lack of fiber.
As the primary food source for gut bacteria, fiber is one of our most important – and in my opinion, most overlooked – nutrients essential for daily consumption.
It’s hard to point to only one culprit because it is the constellation of a SAD that makes it detrimental to gut health. The variables just listed provide food for the growth of undesirable bacteria and ever decreasing numbers of healthy gut flora.
To be fair, this is not just an American problem. These dietary trends are seen all over the world. Many – especially developed – countries around the world are at risk of intaking a diet low in whole foods, fiber, and high in nutrient poor processed foods. It is a broader cultural dilemma of our increasingly fast-paced, grind culture of Western-style capitalism and convenience.
Antibiotic Use
Antibiotic use is probably the most well-known of the causes and contributors to dysbiosis. If you have dysbiosis, there is quite possibly either a history of a great deal of antibiotic use, or one or two rounds of a very potent, broad spectrum antibiotic.
Repeated use of antibiotics is oftentimes in childhood, but many adults have had repeated courses of antibiotics for things like recurrent sinus infections or other infections that haven’t had a root cause approach.
These infections can get bad and create a lot of suffering on their own. Dysbiosis resulting from these powerful antimicrobial treatments then takes an already dysfunctional system to a new level of trouble.
Antibiotics don’t just kill pathogens, or the “bad bugs”. They typically kill many other bacteria, including healthy bacteria you require for normal gut physiology.
In case you think I may have a bias here since I have my degree in naturopathic medicine – let me emphasize that I am a naturopathic, functional and integrative physician.
Being integrative means I see where every medicine has its place. I’m not against antibiotics in any dogmatic sense. I know they have an important and sometimes life-saving role, and I have prescribed them when I thought they were the best option.
However, it is vital as doctors and patients that we understand the true strength and impacts of pharmaceutical antibiotics when making healthcare decisions, so as not to go against what for us as naturopathic doctors is the first principle – First Do No Harm.
Other Medications
Many medications impact the microbiome in a negative way. Each of these medications has its own mechanisms by which it does this. These will not be covered here, but this is a list of common medications from the peer reviewed literature that can potentially lead to, or maintain dysbiosis.
- Proton pump inhibitors (PPI)
- Non-steroidal anti-inflammatory drugs (NSAIDS)
- Metformin
- Opioids
- Statins
- Levothyroxine (T4)
- Psychotropics
- Phloroglucinol
- Anti-vitamin K anticoagulants
Chronic Stress
Chronic, unmanaged stress has one of the worst impacts on your gut integrity and overall health. Stress is not inherently an issue. In fact, it’s often beneficial. The key is that we appropriately adapt to stress.
When stressors pile up and are present for a long period of time, our body and mind’s ability to cope and adapt can become dysfunctional. Stressors can be physical or mental/emotional.
Excessive worry, prolonged unprocessed grief, financial troubles, divorce, and environmental toxicity are a few real life examples I have seen in my practice.
Any time there is a chronic illness or chronic inflammation, there is a reasonable chance that the stress response systems are becoming taxed. The hypothalamic-pituitary-adrenal (HPA) axis is a primary system involved in adapting to stress.
These chronically heightened and maladaptive stress responses lead to a number of gut problems, including:
- Dysbiosis
- Intestinal Permeability (Leaky Gut)
- Immune System Suppression and Dysregulation
- Compromised Digestion
- Malabsorption
- Symptoms of Irritable Bowel Syndrome (IBS)
Specific Dietary Factors
Aside from the many issues with a modern, highly processed food diet, there are certain ingredients that are troublesome for gut function.
Emulsifiers disrupt the mucus layer in the intestines by essentially emulsifying the mucus. As one of the most important components of innate immunity, the mucus layer prevents from infection, gut lining inflammation, and the development of intestinal permeability. These shifts may contribute to worsening dysbiosis as well.
In recent years, the realization that many food coloring agents are likely to contribute to dysbiosis and intestinal inflammation has gained a lot of research attention. These two studies (1 ,2) demonstrated the development of colitis in mice exposed to a variety of food dyes, while this 2023 study shows the impacts of food dyes on gut bacteria.
Most of the research has been done on azo dyes.
These include:
- Red 2
- Red 40
- Yellow 5
- Yellow 6
Excessive Hygiene
This point is likely more of a problem in early life. As you will recall, the infant gut gets some bacterial exposure in utero, followed by a large influx of parental and environmental exposure after birth.
Many of the environmental exposures contribute to the composition of our early gut microbiome. These exposures also serve as a primer for our immune systems. Being too clean has been connected to higher incidence of allergies and atopic disease in children.
Alcohol Consumption
Alcohol is a potent disregulator of the digestive system and the microbiome. For relative purposes, you can think of it as the same thing as refined sugar for your gut bacteria. Excessive alcohol consumption has similar effects to sugar, in that you will be promoting overgrowth of less desirable bacteria and possibly a decrease in the numbers of beneficial bacteria.
Excessive alcohol consumption is often a primary contributor to Candida overgrowth.
Alcohol also causes leaky gut and can lead to decreased stomach acid and atrophic gastritis.
Immune Suppression
Anything that suppresses or alters the immune system from a place of balance has the strong potential to cause dysbiosis. The relationship between the immune system and the microbiome is a two-way connection.
While healthy gut bacteria are required for a normally functioning immune system, the reverse is also true. A healthy immune system is required to maintain a balanced microbiome. Without robust immune system function, organisms like Candida and many types of bacteria can overgrow and cause a cascade of health problems.
Chronic stress has already been mentioned as a known immune suppressor. This is truly one of the most insidious and detrimental modulators of the immune system.
Environmental factors play an important role as well. The list of chemicals that may dysregulate the imune system is lengthy. This table lists toxins that may impact the immune system and where they are found.
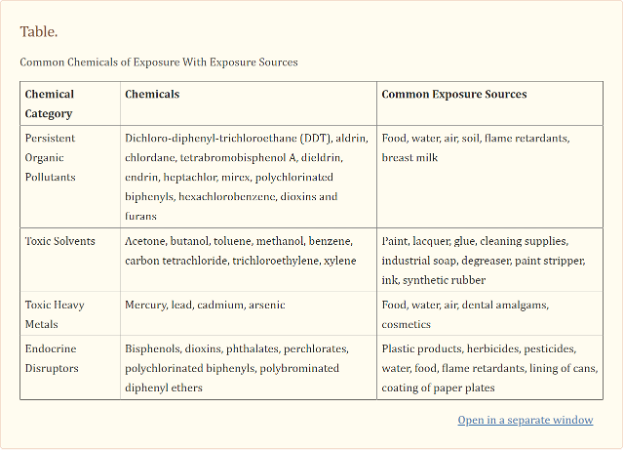
Kharrazian D. Exposure to Environmental Toxins and Autoimmune Conditions. Integr Med (Encinitas). 2021;20(2):20-24.
Certain medications also suppress the immune system. Beyond the list of medications already named that negatively impact gut flora, corticosteroids such as prednisone are potent suppressors of the immune system.
Another important immune suppressant are chronic infections. Of course, an infection like HIV is inherently immune system suppressive. However, any chronic infection your body is battling consistently has the potential to deplete your immune system. This is seen in viral infections for example, where over time the cells that fight viruses known as lymphocytes become depleted and numbers trend low.
Gut Infections
It should be no surprise that if you get an infection that is specific to your digestive tract, it can cause a disruption in the microbial ecosystem. Depending on the pathogen, the alterations in gut flora homeostasis can be severe.
This is evidenced by the fact that ~10% of IBS symptoms begin after a bout of acute gastroenteritis. This could be due to food poisining, for example. Another common infection is from parasites from contaminated water. Giardia and Blastocystis hominis are common examples of these.
In reality, the gastroenteritis could be anything that enters into the system with enough force and influence to significantly disrupt homeostasis. After this, it can be difficult to return to balance and targeted, holistic interventions are often required.
VI. Recognizing the Signs of Dysbiosis
Dysbiosis can result in a number of symptoms both in and outside of the digestive tract. While many of the systemic symptoms may be general, if dysbiosis is a cause, there will usually be some signs in the digestive system.
Digestive Symptoms
Digestive symptoms of dysbiosis can vary from person to person, but common symptoms may include:
- Bloating
- Gas
- Abdominal pain or discomfort
- Constipation
- Diarrhea
- Irregular stool consistency
- Acid reflux or heartburn
- Nausea or vomiting
- Foul-smelling stools
- Unexplained weight changes
These symptoms may occur intermittently or persistently, and their severity can range from mild to severe.
Other Potential Indicators of Dysbiosis
In addition to digestive symptoms, dysbiosis can manifest with various non-digestive system symptoms. These may include:
- Fatigue or low energy levels
- Mood disturbances, such as anxiety or depression
- Difficulty concentrating, or brain fog
- Skin issues, including acne, eczema, or other rashes
- Joint pain or stiffness
- Headaches or migraines
- Allergies and sensitivities
- Autoimmune conditions or flare-ups
- Weakened immune function, leading to frequent infections or illnesses
- Hormonal imbalances, such as irregular menstrual cycles or hormonal acne.
These non-digestive symptoms can occur alongside or independently of digestive symptoms and may vary in severity and duration. It’s important to be aware that dysbiosis can have systemic effects beyond the gastrointestinal tract, impacting various aspects of overall health and well-being.
If experiencing any of these symptoms, seeking medical evaluation is imporant and addressing gut health may be beneficial.
Case Example:
Jennifer was a 60-year-old female who came to see me for what turned out to be the most intense irritable bowel syndrome (IBS) presentation I’ve seen yet. Her case illustrates well how dysbiosis can show up in multiple ways.
Her digestive symptoms included painful gas and bloating that didn’t seem to correlate to any particular foods. When she would bloat the pain was intense enough to put her in bed curled up, ussually for many hours. She also had severe heartburn.
Jennifer would also have pain without obvious bloating, and it usually correlated to bowel movements, which were consistently loose or watery.
This all started after a serious bout of acute gastroenteritis of unknown cause, about 5 years prior. Based on the history, it was likely from contaminated water.
Of note in Jennifer’s case are the many symptoms that were not in the digestive tract. She had severe fatigue that would come in waves and often correlated to her abdominal pain. She would be in bed for days at a time with very low energy. Many times she would have migraines and some form of digestive complaint accompanying the fatigue.
In addition to this, there were periodic waves of joint pains that would last for a couple of weeks to a month at a time. As you can imagine, Jennifer had a great deal of diagnostic workup from many other doctors and specialists prior to seeing me.
She reported to me at the first visit that she only had a few days a month where she was totally functional.
After years of receiving no answers or help, one of the first things we did was a comprehensive diagnostic stool analysis (CDSA), which will be discussed shortly.
What it showed was severe dysbiosis but with no infectious organisms present.
It was a difficult road but with fundamental approaches like those discussed here, and consistent investment in the process, Jennifer was able to greatly improve her total body health. Her digestive tract is still sensitive to certain triggers, but she no longer has symptoms that keep her from living a full life.
IV. Dysbiosis and Its Impacts on Health
Many of the negative health consequences connected to dysbiosis and gut dysfunction have already been alluded to in this article. If you take all of the benefits of a healthy microbiome into consideration and imagine what happens if those roles aren’t being upheld, you can picture what health issues might arise.
Of course, symptoms of dysbiosis can often be troublesome on their own. Worse than the direct symptoms of dysbiosis however, are the potential long term consequences.
The negative health impacts of dysbiosis are far reaching. The list of diseases correlated with dysbiosis and various alterations in the gut microbiome are far too numerous to list and discuss here.
If you search the internet for any condition you are interested in and the microbiome, you are likely to find research connecting the two.
Instead of discussing individual health conditions, I will list some general negative health impacts from dysbiosis. The mechanisms below are why we see the majority of dysbiosis-related chronic illness arise.
Negative Impacts of Dysbiosis
- Intestinal Permeability (Leaky Gut)
- Immune Dysregulation (Autoimmunity, Allergies, Atopy, Asthma, etc.)
- Inflammation (Gut and Systemic)
- Increased Oxidative Stress (Gut and Systemic)
- Leaky Blood Brain Barrier and Neuroinflammation
- Hormonal Dysregulation (ex. Estrogen Dominance)
- Metabolic Irregularities (ex. Insulin Resistance, Weight Loss Resistance or Weight Gain)
- Impaired Detoxification
- Neurotransmitter Imbalance
- Hypothalamic-pituitary-adrenal (HPA) axis dysregulation / Adrenal imbalance
Recognizing and addressing dysbiosis is paramount for maintaining optimal health and preventing the onset of chronic health issues.
In the following sections, I’ll share how to recognize the signs of dysbiosis and implement effective strategies for restoring gut health, permanently.
IV. Diagnosing Dysbiosis
If you are wondering if you have dysbiosis, a conventional medical practitioner will likely not be of much help. Conventional medical practitioners are trained to diagnose common health conditions and infectious diseases, and that is typically where the knowledge base ends.
Unfortunately, when it comes to restoring health in functional illness and supporting the natural healing mechanisms of the body, there is little training among the majority of conventionally trained practitioners.
Functional and naturopathic medicine professionals understand these diagnostic criteria, but importantly, what the underlying triggers and maintaining factors are for disease.
Naturopathic and functional medicine trained doctors have a wealth of guidance to provide and can help you to uncover if dysbiosis is causing your symptoms and contributing to disease.
Luckily, there are some relatively straight forward testing options to evaluate for dysbiosis.
Medical Tests
There are two tests that will give you the most information about gut health and the status of your microbiome. One is a comprehensive diagnostic stool analysis (CDSA) and the other is an organic acids test (OAT).
CDSA
Comprehensive Diagnostic Stool Analysis is available through many different private lab companies. These tests will typically analyze a stool sample for a multitude of different organisms, both healthy and pathogenic, as well as a variety of markers of microbiome health and functional digestive status.
The microbial sections are usually broken up into a few different categories.
- Commensal (healthy) Bacteria
- Potentially Pathogenic Bacteria (Only a problem if overgrown)
- Pathogenic Bacteria
- Fungi (Candida and others)
- Parasites (Worms, Protozoa, etc.)
Of course, one benefit of a CDSA is that you can see if there are any acute or chronic pathogenic microbes contributing to your symptoms. From the dysbiosis perspective, the information can be invaluable.
With the reporting of the healthy and potentially pathogenic bacteria, you get a picture of what major groups are low and high. This not only helps you and your practitioner identify if dysbiosis is a problem, but what kind of personalized therapy might be best for you.
Organic Acids Test (OAT)
Organic acids are byproducts of metabolic processes of living organisms. For example, in every one of your cells, your mitochondria produce a variety of organic acids in the process of energy metabolism.
Bacteria and fungi also produce organic acids as metabolic byproducts. An organic acids test (OAT) is a urine test that analyzes the presence and quantities of a variety of organic acids. Some of these are specific to microbes. By seeing how many microbial organic acids are present in your urine and their respective levels, an OAT can give you a good idea of the presence of dysbiosis and possibly inference into the specific types of microbes that are a problem, such as Candida.
Self-assessment Tools for Identifying Dysbiosis
There are no at home tools to definitively say you have dysbiosis. However, there are some ways you can feel relatively confident before you ever get a medical test.
One is based on symptoms alone. If you have certain digestive symptoms, it’s a fair bet that you have some level of dysbiosis that could benefit from addressing. For example, the presence of gas and bloating, constipation and/or diarrhea, digestive discomfort, and foul smelling stools together would make be presume dysbiosis clinically, without even testing.
The fewer digestive symptoms there are, the less clear it is, and the more beneficial testing may be.
Another at home test is to notice changes is symptoms, especially digestive, from changing your behavior. Dysbiotic bacteria or fungi will respond to changes in their food source.
Bacteria love to eat fiber and sugar sources. They ferment these and as a byproduct can produce gas and other byproducts. FODMAPs are dietary carbohydrate sources that are easily fermentable by bacteria. FODMAP stands for fermentable olig-, di-, monosaccharides, and polyols.
If you get an increase in gas, bloating, and abdominal discomfort from eating high FODMAP foods, along with other dysbiosis symptoms, the likelihood of dysbiosis is higher – not guaranteed, but higher.
Candida and many gut bacteria love sugar as a food source, so sugar cravings are very common if you have dysbiosis. In this case, it is literally the microbes telling your brain to eat sugar because they want to get fed. Again, taken with everything else mentioned, this adds another tic mark that dysbiosis may be present.
V. Resolving Dysbiosis: Effective and Holistic Strategies
Are you frustrated with your efforts to improve your digestive health? Have you tried many different approaches, only to find they don’t work as well as you’d hoped or your symptoms return shortly after?
There are a lot of individualized reasons this can happen, and you are not alone. This experience and the frustrations with it are common and are a regular part of what I see in practice.
As a naturopathic doctor with over a decade of clinical experience, I can tell you definitively that a holistic, well-rounded treatment approach based on science is always superior, regardless of health condition or symptom picture. Digestive issues such as dysbiosis are no exception.
Follow these steps and you will see different outcomes than in the past. I can say this confidently because this approach is what I do in my practice that I know works.
If you’ve been having trouble resolving Candida overgrowth specifically, this article explains some of the common reasons why this happens.
Important Questions to Ask Yourself
The first thing to consider when addressing dysbiosis is the initial cause – or perhaps causes.
Ask yourself a few important questions:
- When did this start and why? If you don’t know why, what does your “gut”/instinct tell you?
- Are the reasons I developed dysbiosis still present in my life? (diet, lifestyle, stress, etc.)
- Are there factors present that predisposed me to developing dysbiosis or that may be preventing me from eliminating it? (Look back at the common causes here.)
- Am I willing to put in the effort to change what is in my control for better health?
Question one helps you pinpoint the primary issue(s). This is important primarily to understand if those are still present, which is the purpose of question number two. If initial factors are still present, they are maintaining factors. Even with this powerful, holistic approach, the results you want will be more difficult if the initial reason for developing dysbiosis is still present.
This also includes gut infections where you’re immune system didn’t clear the organism and now you have a chronic infection of your digestive tract.
Question three is similar. If you developed dysbiosis from an antibiotic treatment or after an acute gut infection, it is possible that your system was already primed for a poor result from certain diet, lifestyle, or other factors. It is also possible that those same factors have helped maintain the current situation.
Lastly, be honest with your level of commitment. Are you willing to take supplements but not ready to change your diet yet? Are you willing to invest financially in your health? Can you commit to your chosen approach for the duration of time required?
There’s no right or wrong here. It’s just getting honest with yourself prior so that you don’t take on something you’re not willing to fully commit to and then “fail” in your goals. Honesty will put you in a place of realistic expectation.
That being said, the recommendations here for diet and supplement use alone are so foundational and effective, I’m confident you will find improvement beyond what you’ve experienced before if you can incorporate these.
VI. CanXida’s Holistic Digestive Support Supplement Line
CanXida is in the business of providing the most effective and unique digestive system formulations available on the market today. Many supplement companies try to make supplements for everything under the sun, making them “ok” at several things. CanXida takes a different approach…
CanXida focuses on one area (the digestive system) intently – making them the world’s leading expert in tailored solutions for the most common digestive system issues facing people today.
This is why I choose to work with CanXida and their supplements when it comes to issues such as dysbiosis, SIBO, and Candida overgrowth.
CanXida Remove Formula RMV
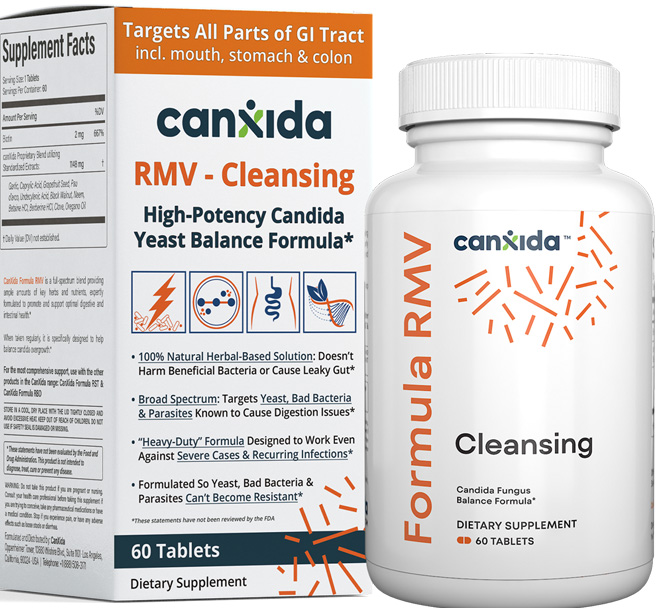
CanXida Formula Remove (RMV) is an all-natural, high-potency, broad spectrum formula that cleanses a broad range of fungi, bad bacteria, and parasites from your gut.
The most common dysbiosis patterns involve several undesirable bacteria present at high levels and sometimes other very bad microbes as well.
This makes it difficult for the good bacteria to gain ground, as the bad guys take up too much space and resources for them to grow.
CanXida Formula RMV cleanses your system in a natural but powerful way. By providing a holistic blend of herbal extracts and naturally occurring plant-derived organic acids, the broad range of bad microbes that can be present in your gut don’t stand a chance.
Beyond the ability to help your body with bad bacteria, parasites, and fungi, this holistic formulation also makes microbial resistance difficult. This is because each of these ingredients acts in different ways and makes development of resistance harder because there are so many targets.
By cleansing your gut of troublesome bacteria, your healthy gut bacteria can begin to take over, especially with the support of the rest of this protocol.
How To Take CanXida Remove Formula RMV:
Any time you start a new supplement with the level of strength as this, it is generally a good idea to start slowly.
For most people, I recommend starting with 1 tablet, once a day with food. If you feel good on that dose, then increase to 2 tablets a day for 7 days. After this, increasing to anywhere from 3-6 tablets a day may be beneficial. It depends on how severe your dysbiosis is and how long it has been present.
2-3 months is a common duration for this formula. Some folks feel better very fast, while some will continue with this formula for 6 months. It again depends on the above factors, as well as if you are doing the rest of the recommendations here.
You can order CanXida Remove by clicking here.
CanXida Restore Formula RST
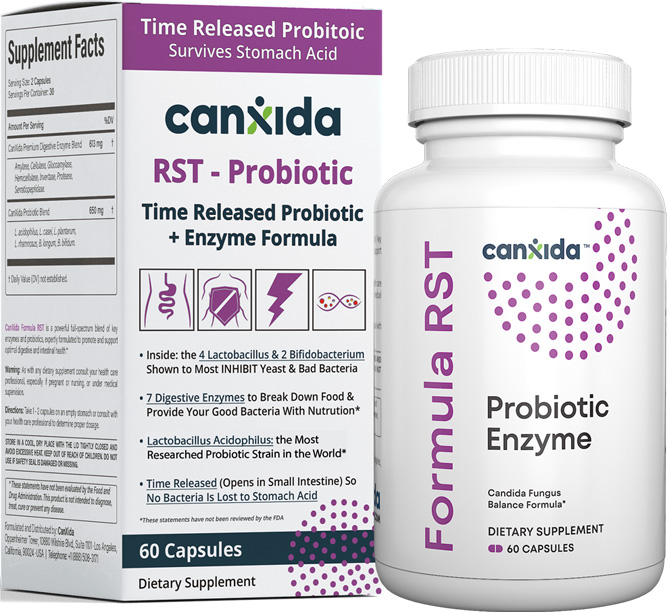
CanXida Formula Restore (RST) is one-of-a-kind digestive enzyme and probiotic blend that helps replenish good gut bacteria as you simultaneously cleanse out the bad ones.
Poor digestion and absorption are common with dysbiosis. CanXida Formula RST gives a healthy dose of digestive enzymes that help your body break down fundamental nutrients into components that are ready for digestion and assimilation.
Another benefit is that pancreatic enzymes, such as those used here, are anti-fungal in nature, which is helpful if Candida overgrowth is an issue for you.
The other game-changing aspect of Formula RST is the probiotics. What you may notice if you compare this to most other probiotic formulas is the difference in the number of strains.
Most probiotics have many different probiotic strains, whereas CanXida Formula RST has only 6 strains. At first thought, this may seem inferior – but here’s the secret…
The strains in RST are the most common and well researched probiotic strains available. While there may be hundreds of different types of bacteria in your gut, those in RST occur in great abundance. When these bacteria increase, colonization and takeover of other bad bacteria also becomes more difficult.
How To Take CanXida Restore Formula RST:
Take one capsule, twice a day. Take the morning dose with food. If you are struggling with Candida, I recommend taking the second daily dose without food.
If Candida is not your issue and it’s a more straightforward bacterial dysbiosis, this is less important but may be worth trying anyway as the enzyme serratiopeptidase does some special things, like balancing inflammation and breaking down biofilms, that may work better on an empty stomach.
CanXida Formula Restore is recommended for a minimum of 3 months.
You can order CanXida Restore by clicking here.
CanXida Rebuild Formula RBD

CanXida Formula Rebuild (RBD) is a high dose multivitamin in combination with ingredients for functional digestive system support.
Nutrient deficiencies are increasingly common today and may be worsened by dysbiosis. Replenishing these commonly missing vitamins and minerals is crucial to a full, healthy functioning immune system.
Every cell in your body requires B-vitamins and antioxidants like vitamin A, D, E, C, selenium, and zinc. These nutrients and more are required for normal cellular function.
CanXida Formula RBD provides a high dose of the most important vitamins and minerals to help replete nutrient deficiencies. This foundational support gets your immune system working on all cylinders and adds another natural support to your body’s own healing mechanisms.
Your body knows how to heal better than anything or anyone else. The best way to support this innate capability is to provide it with the necessary nutrients to do what it knows best.
Lastly, CanXida Formula RBD contains a unique blend of herbal extracts and other natural ingredients such as Betaine HCL, that support the normal function of multiple areas of your digestive tract and give an additional microbial cleansing boost.
How To Take CanXida Rebuild Formula RBD:
Take one tablet twice a day or two tablets once a day with food.
My recommendation is to first use this formula and after a couple of months, replace it with CanXida ReCharge Formula RCH. (This formula is discussed next.)
If you choose to not switch to CanXida Formula ReCharge, it is wise to remain on this supplement for at least 3 months.
You can order CanXida Rebuild by clicking here.
CanXida ReCharge Formula RCH

CanXida Formula ReCharge is a nutrient dense, gut repair dietary supplement. It provides a truly holistic blend of digestive tract healing nutrients with a meaningful dose of the most important nutrients for sustained daily energy and cellular healing.
While Rebuild is meant to replenish depleted nutrient status, ReCharge is meant for nutrient maintenance. The doses of each vitamin and mineral are lower for this reason, which leaves room for the gut repair aspect of the ReCharge formula.
With potent antioxidants and inflammation modulating plant extracts, damage to the gut lining is quenched and prevented from recurring. Targeted amino acids provide energy for cells of the intestines, helping them regenerate and seal up a leaky gut.
Of course, all that work you did to build a healthy gut microbiome needs continued support. So, CanXida Formula ReCharge contains a potent prebiotic food for building and maintaining healthy gut bacteria – Larix laricina (Larch) heartwood extract.
How To Take CanXida Formula ReCharge:
1 scoop a day in water or a smoothie. It can also be consumed at the same time as other food or on its own.
If you were taking CanXida Formula Rebuild prior, be sure to stop it when starting ReCharge, as the dose of certain nutrients could become too high.
This formula can be taken long term for continued gut health support.
You can order CanXida ReCharge by clicking here.
Dr. Blake’s Recommendation
Restoring health and living a new life with less limitations takes investment. It takes the investment of energy, time, intention, and discipline to do things differently.
This is a conversation I regularly have with my patients (and myself when trying to make a meaningful change).
Whether paying to get expert advice, or for professional grade supplements to specifically address your health needs, financial investment is often required as well.
When I need to invest in my health, here’s the way I think of it:
“What’s the cost if I do nothing?” “How will I feel in a year, or two, if I do nothing right now?”
Cost doesn’t just mean money. Will I miss time with my family? Or doing things that bring me joy? Will I miss work due to symptoms? Etc. I consider all these factors and more.
If you are resonating with the information I’m sharing here, it is time to invest in your health.
CanXida has some great savings on packages of the supplements discussed here.
These are a few of my favorite bundles:
VI. Dysbiosis Diet
Just as diet can contribute to developing dysbiosis, it is also foundational to reversing it. My goal with dietary interventions is to always add in as much as possible and restrict as little as possible. Nourishment is the goal.
Many folks on the internet and even practitioners will give very restrictive diets. Sometimes many whole categories of foods will be eliminated, which not only makes eating unenjoyable over time, but can lead to nutrient deficiencies and disordered eating. In most cases, overly restrictive dietary approaches are not necessary to overcome dysbiosis.
Food sensitivities and intolerances do need to be addressed and will be discussed. However, as a general rule, you can follow these simple tenets.
- Whole Foods
- Nutrient Dense
- Variety
- Majority Plants
As simple as that sounds, it covers exactly how you need to eat to overcome dysbiosis.
If you are used to eating a lot of packaged and processed foods, eating only whole foods or things that are minimally processed can feel very restrictive at first. It takes some getting used to but what you will find is that your diet will become more and more expansive as you incorporate more new foods.
The Standard American Diet (SAD) and similar diets are actually quite restrictive and contain relatively little diversity. This is an opportunity to make dietary changes that will last for the long term and provide lifelong health.
Avoid Sugar, Alcohol and Refined Carbohydrates
This is the number one avoidance that you need to strive to abide by. These set the stage for the development of dysbiosis and can be a primary maintaining factor.
I don’t personally like the “never” mentality when it comes to food. However, for at least a month I recommend being as strict as possible with these. After that, they should still be very periodic, but going out and having that small treat with your friends or having a couple squares of your favorite chocolate is not going to ruin your progress.
Now, if you eat half the cake, it might set you back a bit but I think it’s also important live your life. Just do it mindfully.
Increase Certain Plant Derived Oils and Proteins
Eat saturated fats and animal protein in moderation. It will be helpful if you increase olive oil, omega-3 fats from walnuts, chia and flax seeds, and plants with other healthy fats like avocados and other nuts. These oils modulate your gut microbiome in a positive way.
Avoid “vegetable oils” such as corn, soy, cottonseed, etc. Also avoid hydrogenated oils and trans fats.
Similarly, plant derived proteins tend to have a favorable effect on the microbiome
Perhaps the most important reason to add more – many more – plants into your diet, is fiber.
Fiber
Fiber is literally food for your gut bacteria and you need to feed them well.
I recommend working toward at least 30g of fiber a day. It may be helpful initially to track your daily fiber for a week to understand your baseline.
If you have a relatively low fiber diet, increase slowly. Increasing fiber too much, too fast, can cause a lot of bloating and discomfort with dysbiosis. The bacteria ferment the fiber and will often produce gas, which can be quite excessive and uncomfortable.
If you have IBS, I recommend increasing fiber very slowly at first due to the presence of visceral hypersensitivity. Try increasing by only 5 g every 5-7 days.
Psyllium husk is a cheap and easy supplemental fiber option that can be helpful in the beginning to increase your fiber intake and also do it in a measured way. I start folks with 5-10g a day, depending on their tolerance.
Do a House “Cleansing”
When starting this whole foods eating journey, you need go through your cupboards, pantry, fridge, freezer, etc., and get rid of all the sweets, baked goods, conventional store bread, packaged snacks like chips, and so on.
If it isn’t a whole food or something non-sugary used in cooking, it generally needs to go.
Be sure and look for sugar in hidden places, such as sauces, dressings, and flavored yogurts.
If it’s in the house, there’s a good chance you’ll eat it at some point. The surest way to avoid these essential dietary removals is to remove them from your home.
FODMAPs
FODMAPs stands for fermented oligo-, di-, monosaccharides, and polyols. These are common components of many different plants and they are highly fermentable. They are great food for healthy bacteria but the strong fermentation can cause a lot of discomfort for some.
Eating a low FODMAP diet for a period of 2-4 weeks can help decrease symptoms associated with functional digestive system disorders. It is commonly used therapeutically for SIBO and IBS for a time for this reason.
It is important to not continue a low FODMAP diet long term as it may contribute to dysbiosis itself by “starving” out good gut bacteria. However, for a short time, this diet can be a bit of a reset.
Many lists of low and high FODMAP foods are available online and there are apps as well.
Elimination Diet
Food sensitivity and intolerances can contribute to intestinal inflammation and leaky gut. Both of these also disrupt the microbiome. Identifying these and avoiding them can make a big difference in your overall health and in overcoming dysbiosis.
An elimination diet is the gold standard for identifying these. Below is the framework for an elimination rechallenge diet. I recommend you do this at some point your gut repair journey. If not right away, it’s worth doing this at some time.
How to do an elimination-rechallenge diet:
- You need to have some kind of symptom(s) that you would like to see improve.
- Eliminate a chosen amount of foods. I usually recommend starting with soy, corn, gluten, potatoes, eggs, and dairy at first. If this is too much, you can do only one food or a few. It’s flexible in that way.
- Eliminate the chosen foods for 3-4 weeks.
- Track if symptoms improved.
- Improvement = an eliminated food is likely contributing; No Improvement = Likley not contributing
- Eat one food on one day. Wait three days as reactions can be delayed. Note any return of symptoms.
- Symptoms return = food triggered symptoms; No symptoms = food likley not related
- Wise to eliminate foods that are found to be triggers for symptoms after the 3 days
VII. Build Vagal Tone
The vagus nerve is often overlooked in combatting dysbiosis. Given that this nerve regulates the majority of your digestive function and impacts the gut microbial milieu, I consider it to be foundational.
There are three ways I typically go about building vagal tone that I will share here.
Digestive Bitters
The vagus nerve innervates a very small portion of the back of your tongue where your bitter receptors also reside.
By placing 5-10 drops of bitter herb tincture on the back of your tongue, you stimulate the vagus nerve. I recommend doing this 4-5 times throughout the day for continued stimulation. Think of it like working out a muscle, only it’s your nervous system.
Taking these 5-15 minutes before meals also supports digestion of food by stimulating digestive juices.
Counseling
This falls under the “managing chronic stress” category. As humans, we are social and communal beings. The healer/patient relationship is a sacred one and is likely as old as our species.
When you are lost, overwhelmed, needing guidance – what do you do? You seek counsel.
Having someone objective who can be a mirror for your experience, provide fresh insights, and sometimes simply be a sounding board, goes miles to help shape your stress response.
I know from personal and professional experience, taking the step to find a counselor you connect with can have profound impacts on your mental and physical health. Give yourself this gift.
Heart Rate Variability Training
Heart Rate Variability (HRV) training is a form of biofeedback. Through learning to breathe in a particular way, you can increase your HRV, and train and balance your autonomic nervous system (ANS).
The ANS is the fight/flight/freeze and rest/digest aspects of your nervous system. Practicing HRV training for 20 minutes a day, five days a week, can strengthen your ANS and vagal tone.
HRV is like lifting weights for your ANS and your vagus nerve.
Search for a biofeedback practitioner or check out a company like HeartMath, who provide HRV apps and devices.
Another option for increasing HRV is to get a device that stimulates your vagus nerve, such as an auricular device.
Case Example:
Shaina was a pale, 16 year old female patient, who’s mother brought her in to see me after many specialist visits and even workup at top medical hospitals.
The story was this…
About every other week, or twice a month on average, Shaina would wake with a severe migraine, nausea, sometimes vomiting, and extreme fatigue. During these episodes, she would be unable to function in her life at all and would have to stay in bed in a dark room.
These were not short episodes. They typically lasted on average 5 days. It was late in the school year when she came to see me and she was in jeopardy of dismissal from school for having so many absences in the year.
This was early on in my practice and I had only been practicing about 2 years. I was taken aback by the intensity of her presentation and felt intimidated at first.
When I took a step back however, I realized what was likely going on and addressed her case from the functional approaches I’ve discussed here.
Shaina needed digestive and microbiome support. We also needed to explore if there were any outstanding food sensitivities present.
I started out with the digestive support. To my astonishment, at the first 6 week follow up, Shaina had a great deal of color in her cheeks. They were red, not pale like the first visit. And she looked more full in her cheeks, in a healthy way.
Most profound was that she had only one bout of her chronic symptoms in the 6 weeks, instead of 3 as she normally would have, and this lasted only a couple of days.
She was doing much better. The next step I wanted was to see if she had a food sensitivity contributing. In fact, she did. When corn was eliminated, she had felt quite well. Upon reintroduction, all of her symptoms returned and were present for 5 days.
This early case taught me the power of foundational and root cause interventions.
VIII. Conclusion
Although you may be dealing with dysbiosis and have tried many approaches, or simply haven’t known what to do about it, you now have a clear template for how to address it based on a naturopathic and functional medicine approach.
The hidden ecosystem of your microbiome can impact every aspect of your health. As a primary regulator of your immune system, hormones, gut-brain axis, digestive function, and nutrient absorption, you don’t want to put off gut and microbiome repair.
Once you recognize dysbiosis and how it’s impacting your health, you are empowered to use the tools I’ve shared here to take your health into your own hands.
Over 10 years of practice, I’ve seen countless people overcome serious digestive and dysbiosis-related health troubles and you can get there too by following the protocol here.
IX. Take Action Now
Here are some useful actions steps you can take now.
Check out CanXida’s free resources.
For ongoing education and expert advice, follow the CanXida YouTube channel.